Device Description and Specification
This section complies with MDR 2017/745 Annex II, Part 1, Section 1.
Product or trade name and general description
Product Name: Legit.Health Plus
Trade Name: Legit.Health Plus
General Description:
| Information | |
|---|---|
| Device name | Legit.Health Plus (hereinafter, the device) |
| Model and type | NA |
| Version | 1.1.0.0 |
| Basic UDI-DI | 8437025550LegitCADx6X |
| Certificate number (if available) | MDR 792790 |
| EMDN code(s) | Z12040192 (General medicine diagnosis and monitoring instruments - Medical device software) |
| GMDN code | 65975 |
| EU MDR 2017/745 | Class IIb |
| EU MDR Classification rule | Rule 11 |
| Novel product (True/False) | TRUE |
| Novel related clinical procedure (True/False) | TRUE |
| SRN | ES-MF-000025345 |
Intended Purpose:
Intended use
The device is a computational software-only medical device leveraging computer vision algorithms to process images of the epidermis, the dermis and its appendages, among other skin structures, enhancing efficiency and accuracy of care delivery, by providing:
- an interpretative distribution representation of possible International Classification of Diseases (ICD) categories that might be represented in the pixels content of the image
- quantifiable data on the intensity, count and extent of clinical signs such as erythema, desquamation, and induration, among others
Quantification of intensity, count and extent of visible clinical signs
The device provides quantifiable data on the intensity, count and extent of clinical signs such as erythema, desquamation, and induration, among others; including, but not limited to:
- erythema,
- desquamation,
- induration,
- crusting,
- xerosis (dryness),
- swelling (oedema),
- oozing,
- excoriation,
- lichenification,
- exudation,
- wound depth,
- wound border,
- undermining,
- hair loss,
- necrotic tissue,
- granulation tissue,
- epithelialization,
- nodule,
- papule
- pustule,
- cyst,
- comedone,
- abscess,
- hive,
- draining tunnel,
- non-draining tunnel,
- inflammatory lesion,
- exposed wound, bone and/or adjacent tissues,
- slough or biofilm,
- maceration,
- external material over the lesion,
- hypopigmentation or depigmentation,
- hyperpigmentation,
- scar,
- scab,
- spot,
- blister
Image-based recognition of visible ICD categories
The device is intended to provide an interpretative distribution representation of possible International Classification of Diseases (ICD) categories that might be represented in the pixels content of the image.
Device description
The device is a computational software-only medical device leveraging computer vision algorithms to process images of the epidermis, the dermis and its appendages, among other skin structures. Its principal function is to provide a wide range of clinical data from the analyzed images to assist healthcare practitioners in their clinical evaluations and allow healthcare provider organisations to gather data and improve their workflows.
The generated data is intended to aid healthcare practitioners and organizations in their clinical decision-making process, thus enhancing the efficiency and accuracy of care delivery.
The device should never be used to confirm a clinical diagnosis. On the contrary, its result is one element of the overall clinical assessment. Indeed, the device is designed to be used when a healthcare practitioner chooses to obtain additional information to consider a decision.
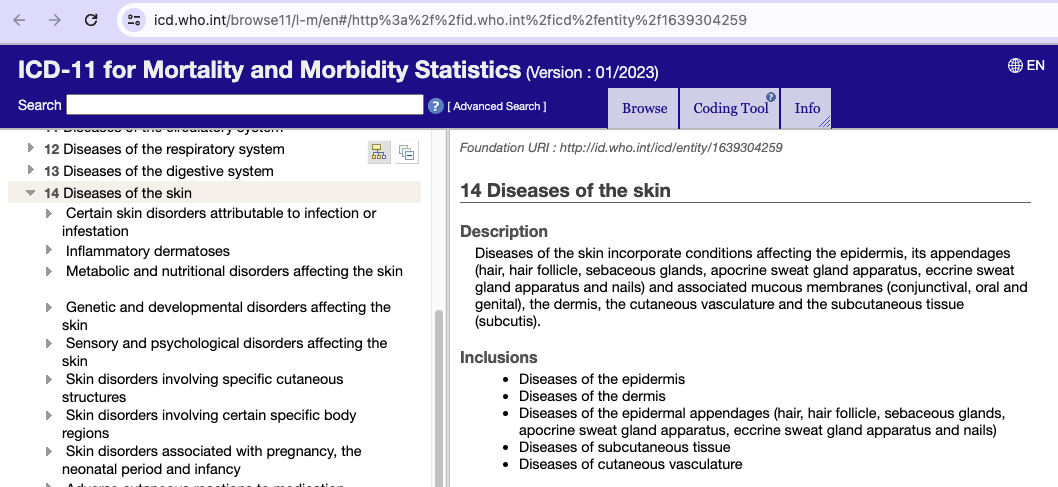
Intended medical indication
The device is indicated for use on images of visible skin structure abnormalities to support the assessment of all diseases of the skin incorporating conditions affecting the epidermis, its appendages (hair, hair follicle, sebaceous glands, apocrine sweat gland apparatus, eccrine sweat gland apparatus and nails) and associated mucous membranes (conjunctival, oral and genital), the dermis, the cutaneous vasculature and the subcutaneous tissue (subcutis).
Intended patient population
The device is intended for use on images of skin from patients presenting visible skin structure abnormalities, across all age groups, skin types, and demographics.
Intended user
The medical device is intended for use by healthcare providers to aid in the assessment of skin structures.
User qualifications and competencies
This section outlines the qualifications and competencies required for users of the device to ensure its safe and effective use. It is assumed that all users already possess the baseline qualifications and competencies associated with their respective professional roles.
Healthcare professionals
No additional official qualifications are required for healthcare professionals (HCPs) to use the device. However, it is recommended that HCPs possess the following competencies to optimize device utilization:
- Proficiency in capturing high-quality clinical images using smartphones or equivalent digital devices.
- Basic understanding of the clinical context in which the device is applied.
- Familiarity with interpreting digital health data as part of the clinical decision-making process.
The device may be used by any healthcare professional who, by virtue of their academic degree, professional license, or recognized qualification, is authorized to provide healthcare services. This includes, but is not limited to:
- Medical Doctors (MD, MBBS, DO, Dr. med., or equivalent)
- Registered Nurses (RN, BScN, MScN, Dipl. Pflegefachfrau/-mann, or equivalent)
- Nurse Practitioners (NP, Advanced Nurse Practitioner, or equivalent)
- Physician Assistants (PA, or equivalent roles such as Physician Associate in the UK/EU)
- Dermatologists (board-certified, Facharzt für Dermatologie, or equivalent)
- Other licensed or registered healthcare professionals as recognized by local, national, or European regulatory authorities
Each HCP must hold the academic title, degree, or professional registration that confers their status as a healthcare professional in their jurisdiction, whether in the United States, Europe, or other regions where the device is provided.
IT professionals
IT professionals are responsible for the technical integration, configuration, and maintenance of the medical device within the healthcare organization's information systems.
No specific official qualifications are mandated. Nevertheless, it is advisable that IT professionals involved in the deployment and support of the device have the following competencies:
- Foundational knowledge of the HL7 FHIR (Fast Healthcare Interoperability Resources) standard and its application in healthcare data exchange.
- Ability to interpret and manage the device's data outputs, including integration with electronic health record (EHR) systems.
- Understanding of healthcare data privacy and security requirements relevant to medical device integration, including GDPR (Europe), HIPAA (US), and other applicable local regulations.
- Experience with troubleshooting and supporting clinical software in a healthcare environment.
- Familiarity with IT standards and best practices for healthcare, such as ISO/IEC 27001 (Information Security Management) and ISO 27799 (Health Informatics—Information Security Management in Health).
IT professionals may include, but are not limited to:
- Health Informatics Specialists (MSc Health Informatics, or equivalent)
- Clinical IT System Administrators
- Healthcare Integration Engineers
- IT Managers and Project Managers in healthcare settings
- Software Engineers and Developers specializing in healthcare IT
- Other IT professionals with relevant experience in healthcare environments, as recognized by local, national, or European authorities
Each IT professional should possess the relevant academic degree, professional certification, or demonstrable experience that qualifies them for their role in the healthcare organization, in accordance with the requirements of the United States, Europe, or other regions where the device is provided.
Use environment
The device is intended to be used in the setting of healthcare organisations and their IT departments, which commonly are situated inside hospitals or other clinical facilities.
The device is intended to be integrated into the healthcare organisation's system by IT professionals.
Operating principle
The device is computational medical tool leveraging computer vision algorithms to process images of the epidermis, the dermis and its appendages, among other skin structures.
Body structures
The device is intended to use on the epidermis, its appendages (hair, hair follicle, sebaceous glands, apocrine sweat gland apparatus, eccrine sweat gland apparatus and nails) and associated mucous membranes (conjunctival, oral and genital), the dermis, the cutaneous vasculature and the subcutaneous tissue (subcutis).
In fact, the device is intended to use on visible skin structures. As such, it can only quantify clinical signs that are visible, and distribute the probabilities across ICD categories that are visible.
Explainability
For visual signs that can be quantified in terms of count and extent, the underlying models not only calculate a final value, such as the number of lesions, but also determine their locations within the image. Consequently, the output for these visual signs is accompanied by additional data, which varies depending on whether the quantification involves count or extent.
- Count. When a visual sign is quantifyed by counting, the device generates bounding boxes for each detected entity. These bounding boxes are defined by their x and y coordinates, as well as their height and width in pixels.
- Extent. When a visual sign is quantifyed by its extent, the device outputs a mask. This mask, which is the same size as the image, consists of 0's for pixels where the visual sign is absent and 1's for pixels where it is present.
The explainability output can be found with the explainabilityMedia key. Here is an example:
{
"explainabilityMedia": {
"explainabilityMedia": {
"content": "base 64 image",
"detections": [
{
"confidence": 98,
"label": "nodule",
"p1": {
"x": 202,
"y": 101
},
"p2": {
"x": 252,
"y": 154
}
},
{
"confidence": 92,
"label": "pustule",
"p1": {
"x": 130,
"y": 194
},
"p2": {
"x": 179,
"y": 245
}
}
]
}
}
}
Basic UDI-DI
Basic UDI-DI: 8437025550LegitCADx6X
Alternative identification:
- Product code: Legit.Health Plus v1.1.0.0
- Manufacturer:
Manufacturer data Legal manufacturer name AI Labs Group S.L. Address Street Gran Vía 1, BAT Tower, 48001, Bilbao, Bizkaia (Spain) SRN ES-MF-000025345 Person responsible for regulatory compliance Alfonso Medela, Saray Ugidos E-mail office@legit.health Phone +34 638127476 Trademark Legit.Health
Medical conditions or diseases to be diagnosed, treated, monitored, alleviated, compensated or prevented
The device addresses medical conditions pertaining to ICD-11 code 14 - Diseases of the skin.
As mentioned, the image-based recognition processor provides an interpretative distribution of probabilities of visible ICD categories. In other words, the device does not provide a true positive or true negative for any specific condition, like diagnostic tests. On the contrary, the device provides the full list of ICD categories and the probability distributed across all the categories.
More information regarding ICD categories can be found in the International Classification of Diseases 11th Revision.
Indications for Use
The device provides two types of information to healthcare professionals:
- Severity Measurement: quantifiable data on the intensity, count and extent of clinical signs such as erythema, desquamation, and induration, among others
- Diagnostic Support: interpretative distribution representation of possible International Classification of Diseases (ICD) categories that might be represented in the pixels content of the image
Contraindications
- Skin structures located at a distance greater than 1 cm from the eye, beyond the optimal range for examination.
- Skin areas that are obscured from view, situated within skin folds or concealed in other manners, making them inaccessible for camera examination.
- Regions of the skin showcasing scars or fibrosis, indicative of past injuries or trauma.
- Skin structures exhibiting extensive damage, characterized by severe ulcerations or active bleeding.
- Skin structures contaminated with foreign substances, including but not limited to tattoos and creams.
- Skin structures situated at anatomically special sites, such as underneath the nails, requiring special attention.
- Portions of skin that are densely covered with hair, potentially obstructing the view and hindering examination.
Warnings - Understanding the Nature of Device Output
Critical Understanding:
The device outputs a probabilistic distribution across all ICD-11 categories related to skin diseases. Unlike diagnostic tests (e.g., COVID-19 or HIV tests) that provide binary results (positive/negative), the device provides an array of ICD categories with distributed probabilities.
| Device | Result type | Output |
|---|---|---|
| Diagnostic test | Binary confirmation | Boolean (TRUE/FALSE) |
| Legit.Health Plus | Probabilistic distribution | Array of ICD categories and distributed probabilities |
The device cannot confirm the presence of a condition. This is a fundamental characteristic of its operation. The probabilistic distribution may be concentrated (leptokurtic) or dispersed (platykurtic) across categories, but the output is always a distribution across all ICD categories, never a binary result.
The device serves as a clinical decision support tool that complements healthcare professionals' expertise. Diagnostic decisions remain with the healthcare professional who combines clinical knowledge, patient history, laboratory results, and other sources of information, including the device output.
Principles of operation
The device operates as a cloud-based API (Application Programming Interface) that processes digital images of skin structures using artificial intelligence algorithms, specifically deep learning technologies, to provide clinical decision support to healthcare professionals.
Core Operating Principles:
- Image Reception: The device receives digital images of skin structures through a REST API interface
- Image Quality Assessment: Images are first assessed for quality and domain appropriateness
- AI Processing: Validated images are processed through multiple deep learning models:
- Vision Transformer (ViT) architecture for ICD category recognition
- Object detection models for counting clinical signs
- Semantic segmentation models for extent measurement
- Image recognition models for intensity quantification
- Output Generation: The device generates structured output in HL7 FHIR® format containing:
- Probabilistic distribution across ICD-11 categories
- Quantitative measurements of clinical signs (intensity, count, extent)
Mode of Action:
The device's mode of action is purely informational and analytical. It does not have pharmacological, immunological, or metabolic effects. The device:
- Analyzes visual patterns in digital images using trained neural networks
- Compares observed patterns against learned representations from validated training datasets
- Generates quantitative and probabilistic outputs based on mathematical computations
- Provides information to support healthcare professionals' clinical decision-making
The device does not make autonomous decisions, does not directly interact with patients, and does not replace the clinical judgment of healthcare professionals.
Rationale for qualification as a medical device
According to the definition of medical device established in Article 2 of Chapter I of the Medical Device Regulation (MDR) 2017/745, the device is an instrument, apparatus, appliance, software, implant, reagent, material or other article intended by the manufacturer to be used, alone or in combination, for human beings for one or more of the following specific medical purposes:
- diagnosis, prevention, monitoring, prediction, prognosis, treatment or alleviation of disease,
- diagnosis, monitoring, treatment, alleviation of, or compensation for, an injury or disability,
- investigation, replacement or modification of the anatomy or of a physiological or pathological process or state,
- providing information by means of in vitro examination of specimens derived from the human body, including organ, blood and tissue donations, and which does not achieve its principal intended action by pharmacological, immunological or metabolic means, in or on the human body, but which may be assisted in its function by such means.
Justification:
The device qualifies as a medical device because it is:
- Software intended for medical purposes
- Used for diagnosis and monitoring of diseases of the skin (ICD-11 code 14)
- Intended for use on human beings
- Does not achieve its principal intended action by pharmacological, immunological or metabolic means
Risk class and classification rule justification
Risk Classification: Class IIb
Applicable Classification Rule: Rule 11 (MDR 2017/745 Annex VIII)
Classification according to MDR 2017/745 Annex VIII
In order to find the appropriate risk class for the device according to Medical Device Regulation (MDR) 2017/745, we apply the classification rules from Annex VIII.
Chapter I: Definitions specific to classification rules
First, we must understand the definitions of the terms.
According to the Chapter I of the Annex VIII of the Medical Device Regulation (MDR) 2017/745, the following definitions apply to the medical device:
| # | DEFINITIONS SPECIFIC TO CLASSIFICATION RULES |
|---|---|
| 1 | DURATION OF USE |
1.1 | 'Transient' means normally intended for continuous use for less than 60 minutes. |
| 1.2 | 'Short term' means normally intended for continuous use for between 60 minutes and 30 days. |
| 1.3 | 'Long term' means normally intended for continuous use for more than 30 days. |
| 2 | INVASIVE AND ACTIVE DEVICES |
| 2.1 | 'Body orifice' means any natural opening in the body, as well as the external surface of the eyeball, or any permanent artificial opening, such as a stoma. |
| 2.2 | 'Surgically invasive device' means: (a) an invasive device which penetrates inside the body through the surface of the body, including through mucous membranes of body orifices with the aid or in the context of a surgical operation; and (b) a device which produces penetration other than through a body orifice. |
| 2.3 | 'Reusable surgical instrument' means an instrument intended for surgical use in cutting, drilling, sawing, scratching, scraping, clamping, retracting, clipping or similar procedures, without a connection to an active device and which is intended by the manufacturer to be reused after appropriate procedures such as cleaning, disinfection and sterilisation have been carried out. |
| 2.4 | 'Active therapeutic device' means any active device used, whether alone or in combination with other devices, to support, modify, replace or restore biological functions or structures with a view to treatment or alleviation of an illness, injury or disability. |
2.5 | 'Active device intended for diagnosis and monitoring' means any active device used, whether alone or in combination with other devices, to supply information for detecting, diagnosing, monitoring or treating physiological conditions, states of health, illnesses or congenital deformities. |
| 2.6 | 'Central circulatory system' means the following blood vessels: arteriae pulmonales, aorta ascendens, arcus aortae, aorta descendens to the bifurcatio aortae, arteriae coronariae, arteria carotis communis, arteria carotis externa, arteria carotis interna, arteriae cerebrales, truncus brachiocephalicus, venae cordis, venae pulmonales, vena cava superior and vena cava inferior. |
| 2.7 | 'Central nervous system' means the brain, meninges and spinal cord. |
| 2.8 | 'Injured skin or mucous membrane' means an area of skin or a mucous membrane presenting a pathological change or change following disease or a wound. |
Chapter III: Classification rules
Now that we know the definitions, it's evident that we are a non-invasive device, and also an active device. Now we can go ahead and find the right class by looking at which rules applies best to our case.
Following the classification rules established in Chapter III, we see that indeed our device is best characterised by Rule 11.
First, we look at 4. Non-invasive devices, and we see that:
Rule 1 All non-invasive devices are classified as class I, unless one of the rules set out hereinafter applies.
So we keep reading, and we get to 6. Active devices. There we discard Rule 9 and Rule 10, because none of them describe our device. However, Rule 11 is representative of the device.
Rule 11
Here's what Rule 11 says:
Software intended to provide information which is used to take decisions with diagnosis or therapeutic purposes is classified as class IIa, except if such decisions have an impact that may cause:
- death or an irreversible deterioration of a person's state of health, in which case it is in class III; or
- a serious deterioration of a person's state of health or a surgical intervention, in which case it is classified as class IIb.
Software intended to monitor physiological processes is classified as class IIa, except if it is intended for monitoring of vital physiological parameters, where the nature of variations of those parameters is such that it could result in immediate danger to the patient, in which case it is classified as class IIb. All other software is classified as class I.
Guideline MDCG 2019-11
To help us determine more clearly whether we are class IIa or class IIb according to Rule 11, we also classify the device with the help of guidance MDCG 2019-11 on Qualification and Classification of Software in MDR 2017/745.
Extracted from Annex III - Usability of the IMDRF risk classification framework in the context of the MDR, of
| High Treats or Diagnoses IMDRF 5.1.1 | Medium Drives Clinical Management IMDRF 5.1.2 | Low Informs Clinical Management (everything else) | |
|---|---|---|---|
| Critical IMDRF 5.2.1 | Class III Category IV.i | Class IIb Category III.i | Class IIa II.i |
| Serious IMDRF 5.2.2 | Class IIb Category III.ii | Class IIa III.ii | Class IIa II.ii |
| Non-serious (everything else) | Class IIa Category II.iii | Class IIa II.iii | Class IIa I.ii |
According to the guidance, classification is determined upon two aspects:
- Columns: the significance of information provided by the medical device software to a healthcare situation related to diagnosis or therapy
- Rows: The effect over the state of healthcare situation or patient condition
According to the rationale of Guidance MDCG 2019-11, the risk classification for the device is Class IIa. In the following two sections, we explain in detail why each is the right fit for the device. However, it is worth noting that we have decided to classify the device as Class IIb, even though the guidance suggests Class IIa, because we prefer to err on the side of caution.
Significance of information: medium
The significance of information is medium. The reason is that the device drives clinical management, but does not treat nor diagnose. This can be understood by looking at the document Software as a Medical Device: Possible Framework for Risk Categorization and Corresponding Considerations authored by the IMDRF Software as a Medical Device (SaMD) Working Group.
Driving clinical management infers that the information provided by the SaMD will be used to aid in treatment, aid in diagnoses, to triage or identify early signs of a disease or condition will be used to guide next diagnostics or next treatment interventions:
- To aid in treatment by providing enhanced support to safe and effective use of medicinal products or a medical device.
- To aid in diagnosis by analyzing relevant information to help predict risk of a disease or condition or as an aid to making a definitive diagnosis.
- To triage or identify early signs of a disease or conditions.
That description fit very well with the intended purpose of the device. Thus, the significance of information is medium.
Effect over patient health: serious
The effect over the state of healthcare situation or patient condition is serious. This can be understood by looking at the document Software as a Medical Device: Possible Framework for Risk Categorization and Corresponding Considerations authored by the IMDRF Software as a Medical Device (SaMD) Working Group.
Here's the definition for Serious situation or condition:
Situations or conditions where accurate diagnosis or treatment is of vital importance to avoid unnecessary interventions (e.g., biopsy) or timely interventions are important to mitigate long term irreversible consequences on an individual patient's health condition or public health. SaMD is considered to be used in a serious situation or condition when:
- The type of disease or condition is:
- Moderate in progression, often curable,
- Does not require major therapeutic interventions,
- Intervention is normally not expected to be time critical in order to avoid death, longterm disability or other serious deterioration of health, whereby providing the user an ability to detect erroneous recommendations.
- Intended target population is NOT fragile with respect to the disease or condition.
- Intended for either specialized trained users or lay users.
That description fits the device's intended purpose. The device provides severity measurements for clinical signs (none serious or life-threatening) and probabilistic distribution across ICD categories (not binary diagnostic confirmation for specific conditions).
With that in mind, let's check one by one the requirements specified in IMDRF 5.2.2
| Requirement for IMDRF 5.2.2 | Applicable | Clarification |
|---|---|---|
| Condition is moderate in progression, often curable | TRUE | Across all the ICD categories, all of them are curable and moderate in progression. |
| Condition does not require major therapeutic interventions | TRUE | Across all the ICD categories, none of them requires major therapeutic interventions. |
| Intervention is normally not expected to be time critical to avoid serious outcomes, providing the user an ability to detect erroneous recommendations | TRUE | Across all the ICD categories, only one is time-critical. In other words, only 0,03% of categories are time-critical, but most importantly: the device's purpose is not to determine whether or not that one time-critical condition is present (positive / negative), but to provide an distributions of all ICD categories. |
| Intended target population is not fragile with respect to the disease or condition. | TRUE | Target population is not fragile |
| Intended for either specialized trained users or lay users | TRUE | Intended for specialized trained users |
For that reason, and keeping in mind the intended use of the device, the effect over patient health is serious, but not critical.
As a result, the device should be classified as Class IIa. However, we have decided to classify the device as Class IIb to err on the side of caution.
Conclusion: The device is classified as Class IIb according to Rule 11 of MDR 2017/745 Annex VIII.
Explanation of novel features
The device introduces <strong>moderate novelties with moderate clinical impact</strong> in dermatological practice.
Clinical Novelties:
- Mode of Use: Assessment of skin conditions is performed using AI-powered analysis of digital images rather than solely visual inspection, enabling primary care practitioners to assess conditions with higher diagnostic accuracy
- Treatment/Management Option: Provides reliable non-invasive analysis for benign pathologies, introducing clinical pathways to potentially avoid invasive procedures such as biopsies
- Interaction and Control: Shifts the diagnostic process from purely human assessment to an interaction between practitioners and artificial intelligence analysis
- Clinical Workflow: Assists practitioners in decision-making by providing additional clinical information that enables faster diagnosis and improved referral decisions, reducing workload and waiting times
Device-Related Novelties:
- Medical Purpose: Addresses previously unmet medical needs in the diagnosis of rare dermatological conditions (e.g., Generalised Pustular Psoriasis, Pemphigus Vulgaris, Palmoplantar pustulosis) where reliable and objective diagnostic tools are scarce
- Design: Novel AI algorithms trained to provide physicians with additional information about suspected diagnosis, disease severity, and referral prioritization:
- Vision Transformer (ViT) architecture adapted for dermatological images
- Multi-modal analysis combining object detection, semantic segmentation, and image recognition
- Model calibration using temperature scaling for interpretable probability distributions
- Test-time augmentation for enhanced prediction stability
- Dermatology Image Quality Assessment (DIQA) for specialized quality control
- Domain verification for automated image validation
- Components: Proprietary AI algorithm constitutes the core innovative component, custom-trained on 181,591 dermatological images to achieve specific clinical performance for the intended medical purpose
Conclusion:
The device introduces moderate novelties with moderate clinical impact in dermatological practice. It offers a new AI-powered methodology that provides additional clinical information to healthcare professionals, improving diagnostic accuracy and clinical workflow. However, it does not introduce new treatment approaches, modify standard clinical procedures, or create new medical intervention categories. The device acts as a clinical decision support tool that complements existing diagnostic methods (visual examination, dermatoscope, biopsies) without replacing clinical judgment.
For complete novelty analysis, refer to R-TF-015-001 Clinical Evaluation Plan Legit.Health Plus.
Accessories and other devices for combined use
The device is accessed via API (server-to-server) and does not require direct accessories.
Healthcare organizations may integrate the device with their Electronic Health Records (EHR) systems. Image capture requires a minimum 12 MP camera.
Note: None of these components are medical devices manufactured by Legit.Health.
Configurations and variants
The device does not have any configurations or variants. It is provided as a single, unified software solution accessible via API.
Key functional elements and composition
General Description of Key Functional Elements
The device comprises the following key functional software components:
- API Interface Layer: REST API implementing OpenAPI Specification with HL7 FHIR® data structures
- Image Quality Assessment Module (DIQA): EfficientNet-based model for assessing image quality
- Image Domain Check Module: Lightweight Vision Transformer for verifying image domain appropriateness
- ICD Category Recognition Module: Vision Transformer (ViT) architecture for probabilistic ICD-11 classification
- Clinical Sign Quantification Modules:
- Object detection models (for counting clinical signs)
- Semantic segmentation models (for extent measurement)
- Image recognition models (for intensity assessment)
- Post-processing Layer: Temperature scaling for model calibration and test-time augmentation
Architecture Diagram
Software Components and Technologies
- Programming Languages: Python (primary), with supporting technologies
- Deep Learning Framework: PyTorch
- API Framework: REST API with OpenAPI Specification
- Data Format: HL7 FHIR® for interoperability
- Model Architectures:
- Vision Transformer (ViT) for image recognition
- EfficientNet for quality assessment
- YOLO-based architectures for object detection
- U-Net variants for semantic segmentation
Software of Unknown Provenance (SOUP)
The device incorporates various third-party software libraries and frameworks, all of which are documented and managed according to the SOUP management plan outlined in GP-012 Design, Redesign and Development.
Raw materials
Not Applicable: As a pure software medical device, there are no physical raw materials, components making contact with the human body, or materials involved in extracorporeal circulation.
The device processes digital image files but does not incorporate physical materials.
Technical specifications and performance attributes
Performance Attributes
The relevant performance attributes are:
| Metric | Value |
|---|---|
| Weight | 33 kilobytes |
| Average response time | 1400 miliseconds |
| Maximum requests per second | no limit |
| Service availability time slot | The service is available at all times |
| Service availability rate during its working slot (in % per month) | 100% |
| Maximum application recovery time in the event of a failure (RTO/AIMD) | 6 hours |
| Maximum data loss in the event of a fault (none, current transaction, day, week, etc.) (RPO/PDMA) | None |
| Maximum response time to a transaction | 10 seconds |
| Backup device (software, hardware) | Software (AWS S3) |
| Backup frequency | 12 hours |
| Backup modality | Incremental |
| Recomended dimensions of images sent | 10,000px2 |
Technical Specifications
API Specifications:
- Protocol: REST API
- Authentication: API key-based authentication
- Data Format: JSON with HL7 FHIR® structure
- Documentation: OpenAPI Specification (Swagger)
- Endpoint: HTTPS secure connection required
Image Input Requirements:
- Minimum Resolution: 12 MP (megapixels)
- Supported Formats: JPEG, PNG
- Color Space: RGB
- Quality Requirements: Assessed automatically by DIQA module
Output Specifications:
- ICD Categories: Probabilistic distribution across 239 ICD-11 categories
- Clinical Signs: Quantitative measurements (intensity 0-10 scale, count, extent in cm² or %)
- Response Time: Typically < 5 seconds per image (depending on network and processing load)
- Data Standard: HL7 FHIR® compliant
System Requirements (for integration):
- Network: HTTPS connection
- Integration Methods: JSON-only, Deep link, or Iframe
- Compatibility: Platform-independent (any system capable of HTTP requests)
Expected Lifetime:
The expected operational lifetime of the device is established at 5 years, which is subject to regular software updates and the lifecycle of the integrated components and platforms. The lifetime will be increased in equivalent spans as the design and development continues and maintenance and re-design activities are carried out.
This timeline accounts for the expected evolution of the underlying operating systems and tools, the progression of medical device technology, and the necessary update cycles to maintain security and operability.
Maintenance and Updates:
- Software Change Management: Regular updates as per
GP-023 Change control management - Security Updates: Ongoing cybersecurity management per
SP-012-002 Cybersecurity and Transparency Requirements - SOUP Management: Continuous monitoring per
GP-012 Design, Redesign and Development
Integration
The device is implemented as an API that integrates with healthcare IT systems (e.g., Electronic Medical Records). Integration allows real-time transmission of dermatological images and reception of clinical assessment data.
Integration Methods
Integration requires IT support. Available methods:
- JSON-only: Direct API integration with POST requests
- Deep link: Integration using pre-designed interfaces and SDKs
- Iframe: Minimal integration embedding pre-designed interface
For detailed specifications, refer to Legit.Health Plus_IFU.
Reference to previous and similar generations
Previous generations
Previous Generation: Legit.Health (legacy device)
The predecessor of the current device is Legit.Health (the "legacy device"), which has been commercialized since 2020 after obtaining the manufacturing license in Spain and was certified under the Medical Devices Directive (MDD) 93/42/EEC as a Class I device.
Similar devices on the market
The clinical evaluation plan identified several AI-based medical devices available on the EU and international markets for dermatological applications. The state-of-the-art analysis revealed that most commercially available devices focus on specific conditions (particularly melanoma and skin cancer detection), whereas Legit.Health Plus offers comprehensive coverage of 239 ICD-11 categories, dual functionality (diagnostic support and severity quantification), and multi-modal AI analysis with seamless EHR integration.
For complete state-of-the-art analysis including identified similar devices, equivalence assessment, vigilance database searches, and clinical performance comparisons, refer to R-TF-015-011 State of the Art Legit.Health Plus and R-TF-015-001 Clinical Evaluation Plan Legit.Health Plus.
Additional Regulatory Information
RDC 751/2022 🇧🇷 - Brazilian Regulation
The device also complies with Brazilian regulation RDC 751/2022.
Justification as a Medical Device
According to the definition of medical device established in Article 2 of Chapter I of RDC 751/2022, a medical device is defined as a product intended for use in humans for purposes such as diagnosis, prevention, monitoring, treatment, or relief of diseases, injuries, or disabilities.
The device meets this definition because it is intended for diagnosis and monitoring of skin diseases (ICD-11 code 14).
Classification According to Risk
According to Rule 11 of RDC 751/2022, software providing information for therapeutic or diagnostic decision-making is classified as Class II. The device matches this rule and does not meet the exceptions that would elevate its classification:
a. Death or irreversible deterioration of a person's state of health (Class IV) b. Serious deterioration of a person's state of health or surgical intervention (Class III)
The device provides diagnostic support but does not replace established gold standard techniques (e.g., biopsies for melanoma). Final diagnostic decisions remain with healthcare professionals.
Clinical Benefits
The device provides clinical benefits by enhancing the precision and efficiency of dermatological assessments through advanced image analysis of visible skin structures. Seven intended clinical benefits have been identified and validated through clinical investigations:
- Improved Diagnostic Accuracy: The device improves accuracy of healthcare providers during the diagnosis of dermatological conditions, with positive impact on patient management and outcomes related to diagnosis and monitoring
- Reduced Waiting Times: The device reduces waiting times for skin-related medical consultations by providing additional relevant clinical information to healthcare providers
- Enhanced Referral Precision: The device improves precision during referral decisions, increasing the adequacy of referrals and positively impacting patient management
- Malignancy Detection Support: The device improves accuracy during diagnosis of lesions suspicious for skin cancer, with positive impact on reducing unnecessary invasive procedures
- Rare Disease Diagnostic Support: The device improves accuracy during diagnosis of rare dermatological diseases, especially benefiting patients suffering from rare conditions
- Objective Severity Measurement: The device measures disease involvement objectively, quantitatively, and reproducibly, increasing precision during patient monitoring
- Remote Care Enhancement: The device improves accuracy during remote diagnosis and precision during remote referrals, particularly beneficial for teledermatology applications
For detailed information on clinical benefits, means of measurement, magnitude of benefit claimed, and supporting clinical evidence, refer to R-TF-015-003 Clinical Evaluation Report Legit.Health Plus.
Signature meaning
The signatures for the approval process of this document can be found in the verified commits at the repository for the QMS. As a reference, the team members who are expected to participate in this document and their roles in the approval process, as defined in Annex I Responsibility Matrix of the GP-001, are:
- Author: Team members involved
- Reviewer: JD-003, JD-004
- Approver: JD-001